Pregabalin Vs Gabapentin: Key Differences and Choices
How Each Drug Works in the Nervous System
They may seem similar at a glance, but beneath the surface their actions diverge in ways that matter to patients and clinicians. Both are GABA analogues that do not directly activate GABA receptors; they bind the α2δ subunit of voltage-gated calcium channels, reducing calcium influx and release of excitatory neurotransmitters. Pregabalin shows higher affinity and more predictable CNS penetration; gabapentin relies on a saturable gut transporter so absorption is variable.
Pharmacokinetic differences shape clinical effects: pregabalin is absorbed faster with linear kinetics so dose changes translate predictably, whereas gabapentin's bioavailability falls at higher doses and control can be variable. Teh faster entry of pregabalin means sooner relief for neuropathic flares.
Both drugs can cause dizziness, somnolence and cognitive fog by reducing synaptic excitability, so clinicians balance efficacy and harms. For some patients switching improves tolerability and occassionally restores function.
Comparing Onset Speed and Dosing Convenience

I recall a patient seeking rapid relief; the opening days mattered greatly. Choosing medication blended evidence with lifestyle. Physicians consider onset, dosing frequency, and whether a regimen will realistically suit work, family, and sleep schedules.
Pharmacokinetics tell a story: pregabalin is absorbed quickly with predictable peak levels, often offering more prompt symptom control. Gabapentin's absorption is dose-dependent and less predictable, so clinical effects can take longer and require careful titration.
From a practical angle, pregabalin's linear kinetics allow simpler twice-daily schedules and lower pill burden, which many patients prefer. Gabapentin often needs three daily doses and dose-dependent absorption, complicating adherence and titration for some individuals.
In practice, the Aparent trade-offs hinge on faster relief versus dosing simplicity, cost, and renal adjustments. Patients should recieve clear counsel on expectations, side effects, and realistic schedules so therapy matches daily life and goals.
Effectiveness Across Neuropathic Pain and Seizures
In neuropathic pain, both drugs reduce abnormal nerve firing, but pregabalin often produces faster, more consistent relief in postherpetic neuralgia and diabetic neuropathy. Trials tend to show higher responder rates at therapeutic doses.
For seizures, each medication is typically an adjunct for focal epilepsies; pregabalin's predictable kinetics make dosing adjustments easier, and some studies report improved seizure control compared with older regimens, especially when combined with other antiepileptics.
Effectiveness varies by condition and dose: pregabalin's linear absorption leads to steadier plasma levels and often a quicker clinical response, whereas alternative agents may need higher or more frequent dosing to acheive similar pain reduction.
Clinicians should balance analgesia and side effects; pregabalin may improve sleep and function for many patients, but Occassionally causes troublesome somnolence or dizziness, so close follow-up and shared decision-making help tailor the best choice in real practice.
Side Effects, Tolerability and Patient Quality of Life

A patient recalls the first night on pregabalin, waking less from pain but feeling foggy; clinicians watch for cognitive slowing and drowsiness too.
Adverse reactions vary: weight gain or dizziness are common, yet many tolerate therapy and report better sleep and reduced pain interference daily.
Tolerability differs by dose and person; slow titration helps. Clinicians balance symptom control with aparant functional gains improve day to day life.
Counselling, monitoring and shared decisions allow patients to acommodate tradeoffs; some switch medicines or taper when benefits no longer outweigh bothersome effects daily.
Risks of Dependence, Misuse and Withdrawal Symptoms
A person starting pregabalin may notice relief, but patients should be aware that pleasurable effects can lead to escalation of dose. Clinicians balance benefit with clear monitoring and patient education.
Withdrawal can be abrupt with anxiety, insomnia and flu like symptoms that sometimes occur when stopping suddenly. Careful tapering and follow up effectively reduce risk for most patients.
Shared decision making helps patients weigh benefits, risks and lifestyle impact. Doctors Recomend realistic goals, screen for substance history and arrange follow up and community support to lower potential long term harms.
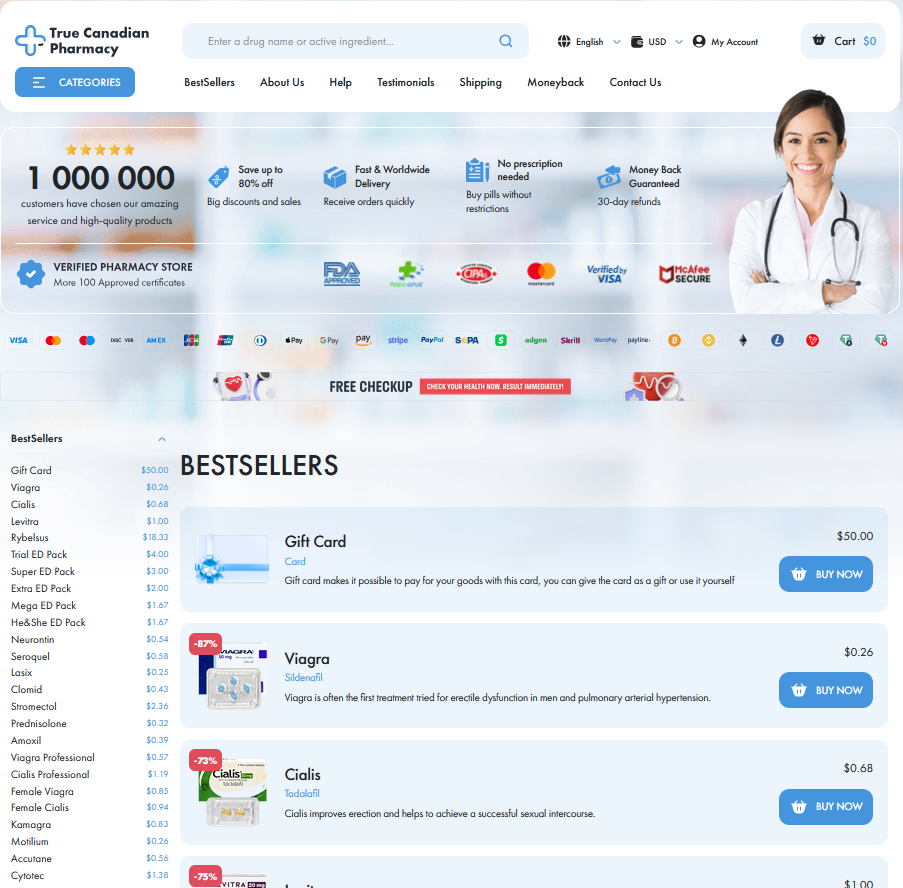
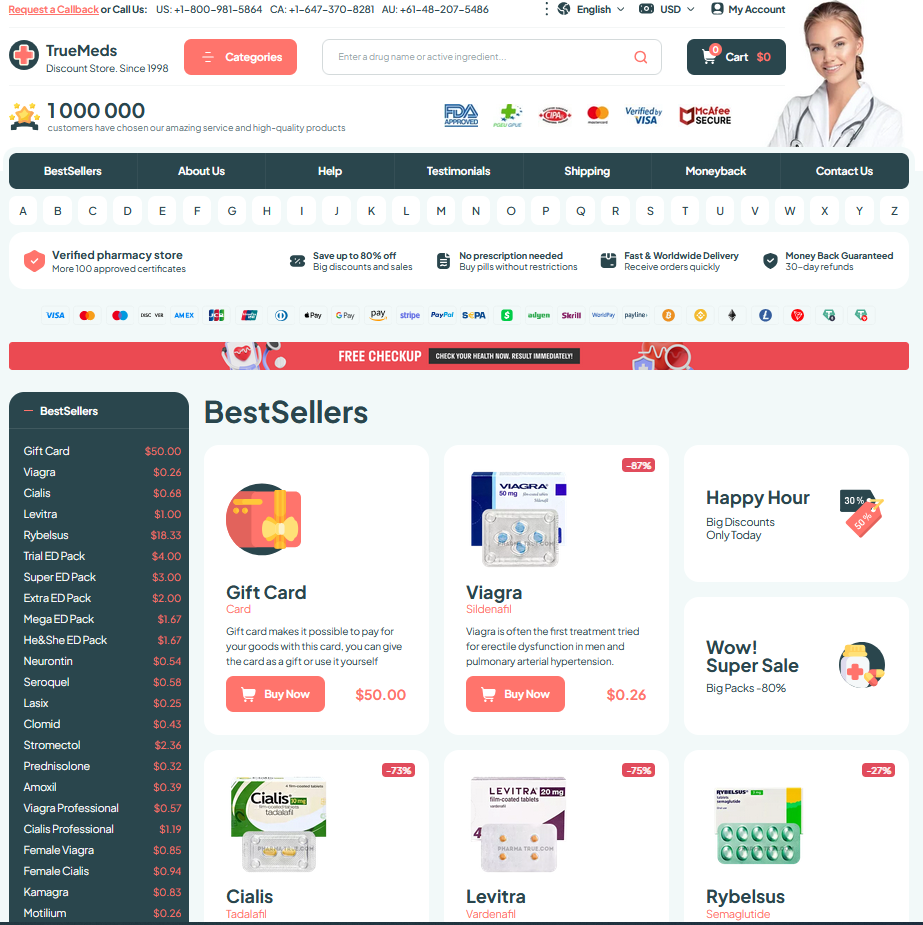
Cost, Accessibility and Practical Prescribing Tips
Out-of-pocket differences can sway choices: gabapentin is usually far less expensive as a long-established generic, while pregabalin often starts as a pricier branded option though generics have lowered costs. Patients should check formularies, seek manufacturer assistance or sample programs, and ask insurers if they will recieve authorization.
Clinicians can balance efficacy, tolerability and access by starting low, titrating slowly, adjusting for renal function, and documenting rationale for choice. Discuss side effects, driving risks and withdrawal planning; coordinate with pharmacists to switch formulations or dose to Acommodate patient finances and adherence. MedlinePlus: Pregabalin EMA: Lyrica (pregabalin)